Introduction
Currently, the scientific literature and available research findings support a strong correlation between positive nutritional status (examples include, not being clinically malnourished, or not losing weight) and better clinical outcomes for patients with cancer, especially among a subset of cancer types (e.g., gastro-intestinal, lung, head and neck) (Isenring et al., 2004; Richards et al., 2020; Wie et al., 2010). Oncology focused Registered Dietitian Nutritionists (RDNs), are nutrition professionals with specialized training to assist patients in maintaining or improving their nutrition status to optimize treatment outcomes. However, for many patients with cancer being treated in the outpatient setting, nutrition services (i.e., RDN care) are not consistently available or accessed (Trujillo et al., 2019). There is a wide range of reasons for this including insufficient staffing of RDNs, misunderstanding the benefit of RDN care, and even the lack of awareness of RDN availability and services (Trujillo et al., 2021).
Dr. Dolores Guest and her staff seek to characterize the availability of outpatient nutrition services for patients with cancer being treated in New Mexico (NM). In this paper, we describe a sub-project of this larger study. We aimed to assess what Outpatient Cancer Facilities (OCFs) publicize on their respective websites in the way of nutrition services available for their patients.
Review of Literature
It is estimated that malnutrition can occur in as many as 80% of cancer patients at some point during or after treatment (Ryan et al., 2016; von Haehling & Anker, 2010). The risk for malnutrition can come from the disease itself or can be a consequence for cancer patients who potentially undergo various treatment plans such as surgery, chemotherapy, radiotherapy, etc. (Platek et al., 2014). Other factors, such as stress, anxiety and depression could also impact nutrition status (Food and Nutrition Board, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine, 2016; Platek et al., 2014). Additionally, the intensity of malnutrition can have a compounding effect given the challenge that not every person who undergoes oncology treatment is well nourished to begin with, resulting in both cancer and cancer treatments aggravating pre-existing nutritional problems (Platek et al., 2014).
We also know that 90% of oncology patients receive treatment in the outpatient setting (Halpern & Yabroff, 2008). This presents a challenge as outpatient cancer settings involves non-standardized screenings. Screenings simply might not be happening, or the use of tools that have not been validated might be utilized, resulting in lack of evidence-based nutritional care (von Haehling & Anker, 2010). Additionally, many patients are not aware of available services (such as malnutrition screening, diet intervention, education, counseling, or nutrition support) if they do not receive direct referrals, such as from a patient navigator (Halpern & Yabroff, 2008). This makes attaining adequate nutrition care for patients challenging as there is currently no standardized way to enforce nutrition guidelines in the outpatient setting compared to inpatient facilities (Thompson et al., 2017).
Methodology Section
To begin characterizing OCF nutritional services, we conducted a descriptive analysis utilizing data collected by searching specific terms on publicly available OCF websites. The goal was to understand what nutrition services are discoverable by a typical patient with internet access. All data searches were conducted in June 2021.
We used two primary sources to identify which facilities to include in our analysis. The first was a list provided by the New Mexico Tumor Registry (NMTR) of the top 20 facilities where tumors were diagnosed in NM (current data from 2013-2018). This list did not include dermatology clinics for two primary reasons: one, many cancers diagnosed at these facilities are treated simply through removal of the cancerous cells and are often low-nutrition risk cancer types. And two the number of cancer diagnoses seen by these facilities in NM is disproportionately high to other cancer types. Indian Health Services (IHS) clinics were also omitted as NM-based IHS facilities do not provide cancer treatment. The second source was the 2021 NM Cancer Council Directory. We further filtered the lists of facilities to only include those that provided treatment in the outpatient setting. Finally, we eliminated any duplicate facilities, which resulted in the final sample size of n=19.
All OCF websites were analyzed with specific search terms to locate any publicized nutritional services offered. We primarily searched on each OCF website’s comprehensive services drop-down tab for services offered, determining if the website had a “Cancer Services”, “Oncology Services”, or “Nutrition Services” tab. If the website did not have those tabs, we utilized the website search bar with the specific terms of “cancer services”, “nutrition services”, or “oncology services” to verify if we discovered any nutritional services through this method. We then kept record of the OCFs that publicized nutritional services on their websites, as well as those that did not.
To provide an understanding of the OCF’s across NM, we categorized the locations of the facilities by NM’s Department of Health public health regions. We documented the number of facilities located in each region, and subsequently the number of OCFs that publicize their nutritional services on their respective websites. Additionally, we took note of the types of nutritional services listed.
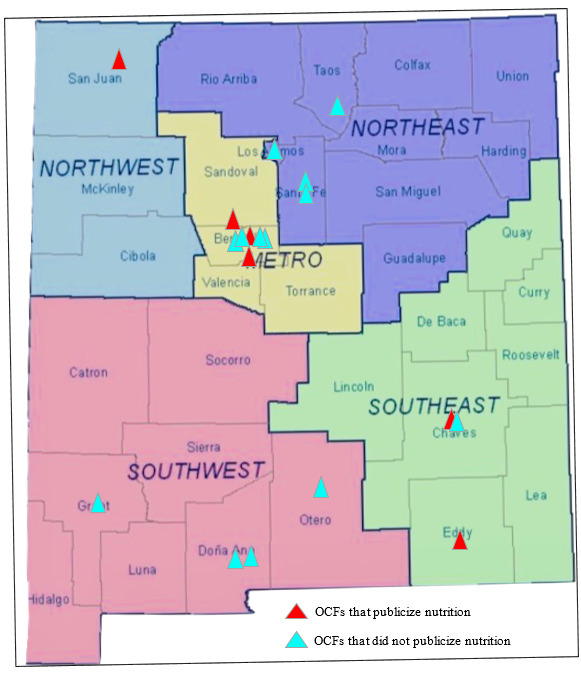
Further, we depicted all 19 OCF facilities on a regional map available on the NM-IBIS website. The red pins represent the locations of the facilities that publicized nutritional services according to their websites, and blue pins represent those that did not.
Results
Six (31.5%) OCFs clearly publicize available nutrition services on their websites (see Table 1). Of these six, half are located in the Metro health region; one (16.7%) is in the Northwest region and two (33.3%) are in the Southeast region (see Figure 1).
The remaining 13 OCFs that did not publicize nutrition services had websites where searches either resulted in zero findings, or it re-directed us to the main home screen of the website.
Discussion
To the best of our knowledge, this is the first study done to analyze nutritional services at OCFs from a patient’s perspective. From the regional map created, most OCFs offering nutrition services are shown to be clustered in a few urban areas. This presents a challenge because NM is predominantly a large and rural state (Caedo, 1974; Herman et al., 2020), which may exacerbate residents access to adequate nutritional care. Additionally, the lack of publicly available information presented by OCF websites may inhibit the confidence of NM residents to navigate the websites and acquire adequate attention for their nutritional health.
Limitations
It is important to note that OCFs may in fact offer nutrition services; however, their websites do not present this information. Additionally, this project is just one perception of navigating nutritional services from a patient perspective and is not inclusive of all avenues to accessing nutrition care. The larger study being conducted by Dr. Guest, along with additional studies will provide additional information crucial to improving provision of nutrition care to people diagnosed with cancer being treated in an OCF. An additional key consideration is that, not all populations within NM will have access to the internet, limiting their access to information through this mode. It is possible that for many patients, they will be made aware of available services only if their oncology providers recognize their individual need for this supportive care and provide a referral, or if the patient themselves seek it out at their treating OCF.
Future Directions
Given the amount of emerging data supporting the importance of nutrition in oncology, my next steps could include surveying and interviewing cancer patients on their experiences accessing nutrition care during and after their treatment to determine their experiences and to what extent additional barriers exist for patients trying to receive adequate nutrition care in NM. Additionally, applying this same patient-perspective approach to compare the NM findings with other OCF’s across the country, could provide important insight into current successes and gaps for patient care. This information would assist in developing necessary, specific interventions to improve awareness of and access to nutrition care for ambulatory oncology patients nationwide.
Conclusion
The findings from this sub-project support the growing body of scientific literature that there is a gap in oncology nutrition awareness and overall utilization. Presently, the availability of diet intervention and counseling services for oncology patients are significantly limited across the state of NM.